Posted on September 2, 2016 by Kristina Swartzendruber , Michigan State University Extension
Diabetes is a disease that affects metabolism and is characterized by high levels of glucose in the blood. Basically, it’s a disease that makes it difficult for the body to turn food into energy. According to the American Diabetes Association, 29.1 million Americans (9.3 percent of the population) had diabetes in 2012. Approximately 1.4 million are diagnosed with diabetes each year.
There are three different types of diabetes:
Type I – Previously referred to as juvenile diabetes, type 1 diabetes can affect anyone at any time but is most prevalent in children, teenagers and young adults. The exact cause of type 1 diabetes is not known, but genetics, environmental influences and other factors may play a role in the development of the disease. Little or no insulin is produced by the pancreas so a person with type 1 diabetes must treat their disease with insulin, diet, exercise and self-management.
Type 2 – Previously referred to as adult-onset diabetes, this is the most common form of diabetes and can affect people of any age but most frequently develops during adulthood. Unhealthy weight, age, family history, lack of exercise and/or a history of gestational diabetes are all risk factors associated with type 2 diabetes. Type 2 diabetes can often be managed with diet and exercise, however, some people may be required to take oral medication and/or insulin.
Gestational – This type of diabetes develops when a woman is pregnant and usually occurs later in the pregnancy. Gestational diabetes usually disappears after the baby is born. Age, family or personal history, unhealthy weight, high blood pressure and/or complications during previous pregnancy are risk factors associated with gestational diabetes. Untreated or uncontrolled blood sugar can cause the fetus to grow very large. Babies born from mothers with gestational diabetes are also at a higher risk of low blood sugar, breathing difficulties and/or jaundice after they are born so it’s very important for women with this condition to work with their doctor to control blood sugar during her pregnancy.
Symptoms associated with all three types of diabetes include increased thirst and urination and/or increased or extreme hunger and fatigue. There are additional symptoms, some of which may go unnoticed, so it’s very important to get regular physicals and communicate with your healthcare professional if you have a family history of diabetes.
Posted on September 6, 2016 by Kristina Swartzendruber , Michigan State University Extension
As a certified trainer for Diabetes PATH, I’ve heard all kinds of myths related to this disease. I still have participants, diagnosed with type 1 or type 2 diabetes, come to the first class believing they can’t eat any of their favorite foods that contain sugar. Some of these myths and misconceptions come from outdated medical practices and information that is not research-based.
According to the American Diabetes Association, diabetes is a serious and potentially deadly disease – myths only create inaccuracy and promote stereotypes and stigma. Below you will find some of the common myths that are found on theAmerican Diabetes Association website paired with relevant facts:
Myth: Diabetes isn’t a serious disease.
Fact: Diabetes affects over 25 million people in the United States and is the seventh leading cause of death in this country. According to the National Diabetes Education Program, your chance of having a heart attack nearly doubles if you have diabetes. Sixty-eight percent of diabetics actually die of heart disease or stroke. The good news is that good diabetic management practices can reduce your risk of complications.
Myth: If you’re overweight or obese, you will eventually develop type 2 diabetes.
Fact: Although being overweight is a risk factor, there are many other risks associated with diabetes such as family history, age, ethnicity, etc. Most people who are overweight never develop type 2 diabetes.
Myth: Eating too much sugar causes diabetes.
Fact: A diet high in calories, from any source, can lead to weight gain which is one of the risk factors associated with diabetes. However, there are many other risk factors associated with this disease, such as a person’s genetics and age. There is research linking the consumption of sugary drinks to diabetes – the American Diabetes Association recommends that we limit our intake of beverages such as regular soda, fruit punch, energy/sports/fruit drinks, etc. to help prevent the onset of diabetes.
Myth: People with diabetes should eat special diabetic foods.
Fact: People with diabetes can generally follow the same healthy meal plan as those without the disease. According to theAmerican Association of Diabetes Educators, it’s important for people with diabetes to eat regular meals, control the amount they eat and make healthy food choices to better manage their disease and prevent other health problems.
Myth: People with diabetes can’t eat sweets, chocolate or starchy foods.
Fact: If sweets and starchy food are eaten as part of a healthy meal plan, or combined with exercise, these foods can be eaten by people with diabetes. There really aren’t any “off limit” foods. The key is to keep track of carbohydrates and watch portion size.
Posted on September 21, 2016 by Kristina Swartzendruber, Michigan State University Extension
Diabetes is a serious disease, affecting nearly 26 million Americans. Traditionally, people who were diagnosed with type 1 and 2 diabetes were prescribed medication, instructed to not eat foods containing sugar and sent on their way. Today, we know that people with this disease can live longer and reduce their risk of some of the complications associated with diabetes, but it takes hard work and cooperation by the person affected. It’s also important for a person to work closely with their healthcare team because the kind of management used depends on the type of diabetes a person has.
Living a Healthy Life with Chronic Conditions offers the following recommendations that focus on the management of diabetes:
Monitoring blood glucose: One of the first goals in managing diabetes is keeping one’s blood glucose levels within a safe range, and the only way to do this is through monitoring. Monitoring should not be considered a treatment but rather a tool that can be used to find out how a person is doing and make the needed day-to-day changes in diet and exercise as well as changes with medication to keep their blood glucose levels at a safe level.
Adopting a healthy eating plan: Eating right is essential to diabetes self-management because in addition to helping maintain normal blood glucose levels, it also can help improve a person’s blood pressure, cholesterol levels and overall health. The good news is that you do not have to go hungry, eat “special foods” or give up your favorite foods if you have diabetes. The main focus should be on meal and snack time planning, portion control and the types of food that is eaten.
Incorporating physical activity: Exercise has many benefits. It can help with lowering blood sugar levels and blood pressure, maintaining a healthy weight, improving cholesterol levels and reducing the risk of heart disease and stroke. Physical activity also helps a person with diabetes use their insulin better. The goal most people should work towards is mild to moderate aerobic exercise 150 minutes a week.
Dealing with stress and emotions: Feelings associated with anger, frustration and fear of the unknown are normal for those dealing with diabetes. Learning various breathing and relaxation techniques may be the first step to dealing with diabetes-related stress. The American Diabetes Association suggests joining a support group where a person can learn from others hints for coping with problems. It’s very important to enlist the help of a doctor and/or therapist if a person’s stress is so severe they are feeling overwhelmed.
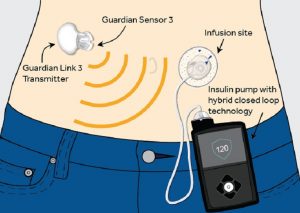
Taking medications: It may be necessary for a person to take oral medication or insulin by injection/pump to help keep their blood sugar levels within a normal range. Again, it’s very important to work closely with a healthcare professional to monitor how your medication affects your blood glucose levels.
Michigan State University Extension offers many disease prevention and management programs that focus on diabetes. For more information, contact your local Extension office.
These articles were published by Michigan State University Extension. For more information, visit http://www.msue.msu.edu. To have a digest of information delivered straight to your email inbox, visit http://www.msue.msu.edu/newsletters. To contact an expert in your area, visit http://expert.msue.msu.edu, or call 888-MSUE4MI (888-678-3464).






 Part 1:
Part 1:  With Type 1 diabetes, the pancreas makes little or no insulin so people have to
With Type 1 diabetes, the pancreas makes little or no insulin so people have to research and talking to people in the diabetes community. We are excited to share what we learned with you here in this space. For our first post, I am going to tell you a little bit about me and why I do this research.
research and talking to people in the diabetes community. We are excited to share what we learned with you here in this space. For our first post, I am going to tell you a little bit about me and why I do this research. communication between parents and their kids. Additionally, with an increase in effective communication, we hope that more trust will be built and the transition to the adolescents’ self-management will be smoother for both the teens and their parents. The content and design of the app was brainstormed by our diverse team of doctors, nurses, and communication researchers. We are currently working with an app development company to create the app. I am fortunate to be working with such talented people on such an important problem. It is my hope that this app will truly make a difference in the lives of families affected by T1D.
communication between parents and their kids. Additionally, with an increase in effective communication, we hope that more trust will be built and the transition to the adolescents’ self-management will be smoother for both the teens and their parents. The content and design of the app was brainstormed by our diverse team of doctors, nurses, and communication researchers. We are currently working with an app development company to create the app. I am fortunate to be working with such talented people on such an important problem. It is my hope that this app will truly make a difference in the lives of families affected by T1D.